- Research
- Open access
- Published:
The impact of eHealth on relationships and trust in primary care: a review of reviews
BMC Primary Care volume 24, Article number: 228 (2023)
Abstract
Background
Given the increasing integration of digital health technologies in team-based primary care, this review aimed at understanding the impact of eHealth on patient-provider and provider-provider relationships.
Methods
A review of reviews was conducted on three databases to identify papers published in English from 2008 onwards. The impact of different types of eHealth on relationships and trust and the factors influencing the impact were thematically analyzed.
Results
A total of 79 reviews were included. Patient-provider relationships were discussed more frequently as compared to provider-provider relationships. Communication systems like telemedicine were the most discussed type of technology. eHealth was found to have both positive and negative impacts on relationships and/or trust. This impact was influenced by a range of patient-related, provider-related, technology-related, and organizational factors, such as patient sociodemographics, provider communication skills, technology design, and organizational technology implementation, respectively.
Conclusions
Recommendations are provided for effective and equitable technology selection, application, and training to optimize the impact of eHealth on relationships and trust. The review findings can inform providers’ and policymakers’ decision-making around the use of eHealth in primary care delivery to facilitate relationship-building.
Background
Primary care is a person’s first point of contact in healthcare systems and includes “disease prevention, health promotion, population health, and community development” ([1, 2] p1). Primary care across the globe is shifting towards team-based models that bring together interprofessional teams of family physicians, nurse practitioners, registered nurses, social workers, dietitians, and other professionals to provide holistic and comprehensive care [3,4,5,6]. These models are designed to address the needs of individuals with multimorbidity and complex conditions in the community as they can offer a diverse skill set to meet the variable needs of this population [7]. Along with an evolution towards team-based primary care models, this past decade has also witnessed an increasing global interest and rapid uptake of digital health in primary care [8,9,10], hastened by the COVID-19 pandemic [11, 12]. Some jurisdictions are considering a “digital-first” primary care model where technology is used as the default care delivery mechanism [13], while others have noted a need to balance appropriate and equitable hybrid care delivery [10].
Digital health broadly refers to the use of technologies for health [14]. Technologies include information and communication technology (also referred to as eHealth), which includes the use of mobile wireless technologies (often referred to as mHealth as a specific type of eHealth) [14]. Digital health technologies can also include emerging technologies, processes, and platforms like big data, genomics, machine learning, and artificial intelligence [14]. eHealth includes: (i) management systems; (ii) communication systems; (iii) computerised decision support systems; and (iv) information systems [15]. The implementation and effectiveness of eHealth is influenced by a complex array of factors and can impact several facets of care delivery [16].
One aspect that can potentially be altered is the nature of relationships and trust between patients and their providers, and within provider teams. Relationships between patients and providers, built on trust, knowledge, regard, and loyalty, have been demonstrated to be fundamental to healthcare delivery [17]. This is particularly important in primary care where patients will tend to have longer-term relationships with their provider or practice [18]. Strong trust-based relationships between providers within teams can enable a positive work environment, improved communication, effective teamwork, and care coordination [19, 20].
eHealth and patient-provider relationships
Patient-provider relationships are often referred to using terms like therapeutic relationship, therapeutic alliance, communication, interaction, and rapport [21,22,23,24,25,26,27]. Trust is thought to be an important component of this relationship [28] and its development has been found to require multiple interactions over time [29]. Promoting trust in the patient-provider relationship includes the demonstration of three key provider attributes: interpersonal and technical competence, moral comportment, and vigilance [30]. Patients perceive trust in providers as linked to their active participation and satisfaction with care [31, 32]. An absence of trust in providers is associated with reductions in treatment adherence and care seeking behaviours by patients, and reduced continuity of care [33] (i.e., connected and coordinated care while moving through the healthcare system) [34].
Trust-based patient-provider relationships are changing with the expansion of eHealth. Henson et al. use the term ‘digital therapeutic alliance’ to refer to patient-provider relationships established through mental health apps [35]. The interconnection between technology and therapeutic relationships is evident in Mesko and Győrffy’s ([36] p2) definition of digital health as “the cultural transformation of how disruptive technologies that provide digital and objective data accessible to both health care providers and patients leads to an equal-level doctor-patient relationship with shared decision-making and the democratization of care”. Studies have reported positive changes accompanying this transformation. Patients may experience greater empowerment through improved access to health information and resources and can assume a more active role in communication and decision-making [36,37,38]. Providers may experience shifts towards empathy-driven care [39], assume the role of a guide to direct patients towards high-quality information and services [36], and support active patient engagement with technology [40]. Some providers value the use of technology for prioritizing patient values, enabling patient autonomy [41], and making caregivers part of the team [42].
However, the impact of technology on relationships has also been termed “a double-edged sword” with significant ethical and safety implications [38]. Technology is thought to harm the relationship and reduce efficiency if patients obtain irrelevant information or misinterpret information [37, 38]. ( For instance, patients may misinterpret data or test results accessed through technology such as self-monitoring devices and smartphone apps when the provider’s involvement is limited) [37]. Patients may also access information through resources on the Internet that may enable them in engage actively in dialogue with the provider but may also lead to them obtaining irrelevant or inaccurate information. Some providers have expressed concerns related to overuse of technology by patients and caregivers (e.g., frequently checking blood sugar or pressure when deemed unnecessary by the provider) [42] and technology taking their attention away from patients during the clinical encounter [41].
eHealth and provider-provider relationships
Relationships between primary care providers that “provide support and sustenance” are among the key factors for compassion among healthcare workers ([43] p123). Like the case of patient-provider relationships, trust is integral to strong team relationships and can contribute to better quality of care and practice improvement through open discussions of successes and failures among team members [23]. In an increasingly virtual care delivery environment, trust-based relationships between providers can facilitate interprofessional collaboration [44]. Interpersonal trust has been identified as a primary determinant of performance in virtual relationships between telemedicine providers [45]. A lack of trust between telehealth nurses and other primary care professionals was found to create tensions in their relationships [37]. The use of health information technology can enhance trust between providers when it facilitates reviewing and affirming non-physician clinicians’ decisions or erode trust when it limits opportunities for developing familiarity and comfort [25].
Objectives and approach
While there is a growing body of literature on the impact of eHealth on patient-provider and provider-provider relationships and trust in primary care, questions remain around how to best integrate eHealth into primary health care systems to facilitate relationship-centred care and uphold the “humanness” of primary care [46]. There is a need to examine this issue to generate specific information that can inform decision- and policymaking around the integration and implementation of eHealth into primary care while considering its impact on relationships and trust.
This paper reports on a review of reviews [47] to synthesise high-level evidence on relationships and trust as related to the use of eHealth in primary care. This approach was selected to identify what is currently known and unknown in this field by summarizing evidence from the large number of existing evidence syntheses, and to generate recommendations on how to ensure eHealth adoption permits and strengthens relationships and trust in primary care. To guide the review, we sought to answer the research question: How does eHealth impact patient-provider and provider-provider relationships and trust in primary care?Given the importance of health equity, especially in relation to the use of digital health in primary care [48], we also sought to understand if eHealth has a differential impact on trust and relationships across different groups (e.g., sociodemographic groups).
Methods
Search strategy
The search strategy was developed for Medline and adapted to EMBASE and Cochrane databases (Additional file 1). Four concepts were included: ‘primary care’, ‘digital health technologies’, ‘relationships’, and ‘trust’. Strategies developed for previous reviews with a librarian’s assistance helped build the search for ‘primary care’ and ‘digital health technologies’. A strategy was developed for the other two concepts (i.e., ‘relationships’ and ‘trust’) using subject headings and non-indexed keywords identified through team brainstorming and literature scans. The initial search was conducted in May 2021, followed by an updated search using the same strategy in June 2022.
Inclusion criteria and study selection
The search focused on peer-reviewed evidence syntheses published in English from 2008 onwards. This timeline was determined based on trends noted in two reviews on digital health in primary care that indicated that most papers were published after 2008 [49, 50]. Included reviews (i) were located in a primary care setting, either exclusively or along with other settings (ii) discussed patient-provider and/or provider-provider relationships and/or trust, and (iii) included the use of digital health/eHealth/mHealth technologies (as defined above, and as consistent with our search criteria listed in search lines 10–25 in Additional file 1) allowing for interaction or information-sharing between patients and providers and/or between providers. As the focus of the review was on adult patients receiving primary care services, reviews exclusively discussing patients below 18 years of age were excluded. Primary empirical studies, conference abstracts, editorials and grey literature were also excluded.
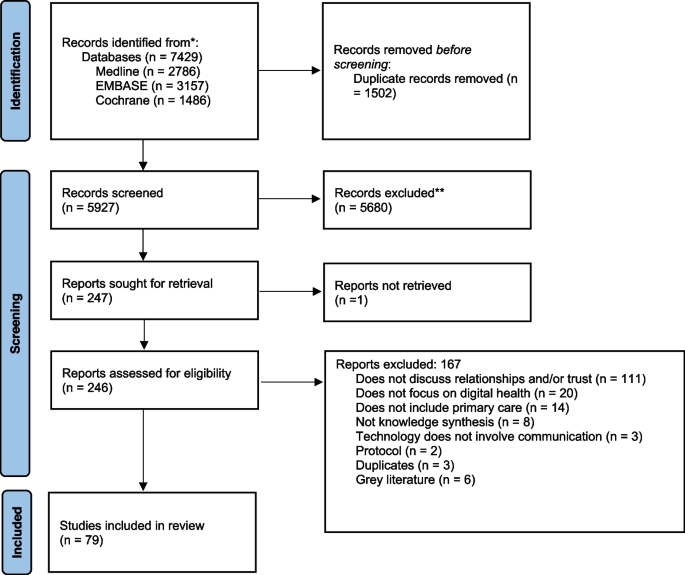
The search results were validated using five articles chosen by the research team that met the inclusion criteria. Articles were then uploaded to EndNote reference manager to remove duplicates, and then transferred to Covidence review management platform for screening. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (Fig. 1) depicts the study selection process. Text screening followed two phases: 1) title and abstract and 2) full text.
-
1)
Title and abstract screening: Two rounds of title and abstract screening tests between three team members were conducted to ensure agreement and alignment with the inclusion criteria at this stage. All three members screened a random sample of 100 titles and abstracts to check if they met the inclusion criteria. Cohen’s Kappa values [51, 52] were calculated between pairs of reviewers (e.g. Rev 1-Rev2; Rev 2-Rev3; Rev 1- Rev3) resulting in Kappa values ranging from 0.496 to 0.754, suggesting moderate to substantial agreement by the second round. Team meetings were held to discuss conflicts, and after the second round it was determined that all three reviewers had come to a common understanding of the inclusion/exclusion criteria to proceed with a single-reviewer approach.
-
2)
Full-text screening: At the stage of full-text screening a single-reviewer approach was deemed sufficient due to clear understanding of inclusion and exclusion criteria established by the reviewers, and due to time and resource constraints..
Data extraction and synthesis
Three members of the research team conducted data extraction. A data extraction sheet was developed for this study and piloted on three articles. It included: type of review; number of studies; research paradigm of authors (e.g., postpositivist, constructionist); study aims; participants; settings; type(s) of technology; definitions of relationships and trust and/or connected terms; factors influencing impact of eHealth on relationships and/or trust; and any discussions around equity (how this impact might differ in different groups).
Based on definitions of relationships from our preliminary literature searches [21,22,23,24,25,26,27], we included reviews directly referring to ‘relationships’ or using other related terms like ‘collaboration’, ‘communication’, ‘connectedness/connection’, ‘interaction’, ‘empathy’, ‘respect’, and ‘understanding’. We searched each included review to see how they had described these terms and then aggregated and analysed these descriptions to identify patterns and interrelationships between terms. We also searched each review for descriptions of the impact of eHealth on relationships and/or trust and classified the impact as positive, negative, or mixed (both positive and negative). When the type of impact was not directly mentioned by the authors, two members of the research team classified the impact based on their interpretations of the authors’ descriptions and following discussions with each other. Technologies were classified using Mair et al.’s four eHealth domains described in Table 1 [15, 53]. Thematic analysis was conducted to determine the impact of different types of eHealth on relationships and/or trust and any influencing factors. Two members of the research team coded data from each article on influencing factors separately. Coding involved highlighting and labelling relevant sections from the extracted data in a Word document. Both members then met to discuss and merge the developed codes into a single document. One member then analysed these codes, and four broad categories were developed (patient-related, provider-related, technology-related, and other factors). The second member then reviewed these categories by checking if they aligned with data extracted from 10 reviews.
Results
Overview of reviews
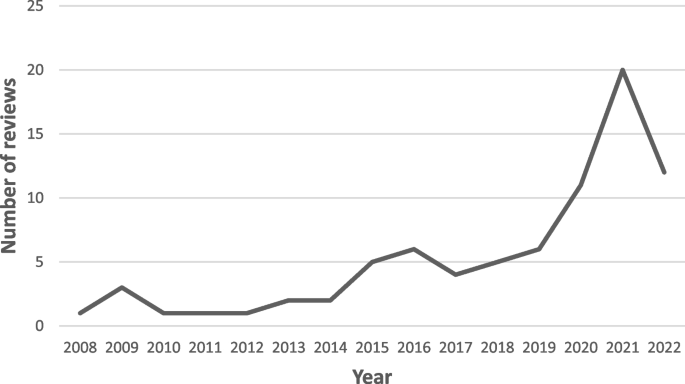
The screening process yielded a total of 79 reviews were included (55 from the initial search and 24 from the updated search). Most reviews were published from 2015 onwards with a notable increase in numbers in 2020, 2021, and 2022 (Fig. 2). Most reviews focused on patient-provider relationships and/or trust (76 of 79), three reviews only discussed provider-provider relationships and/or trust, and 19 reviews focused on both groups. The majority of reviews either focused exclusively on adult patient populations (31 of 79) and providers from multiple disciplines (37 of 79) or did not describe the patient (37 of 79) and provider population (35 of 79). Reviews either exclusively focused on primary care (14 of 79), discussed a range of settings including primary care (40 of 79), or did not clearly describe the settings (25 of 79). Of the four domains of eHealth technology, communication systems were discussed most frequently (38 of 79), followed by reviews discussing multiple types of technology across the four domains (19 of 79) and management systems (17 of 39). Fourteen reviews discussed how the impact of eHealth (mostly communication systems) on patient-provider relationships and/or trust may differ based on age, socioeconomic status, functional ability, language, or being part of a minority/disadvantaged group [16, 54,55,56,57,58,59,60,61,62,63,64,65,66].
Seventeen reviews discussed the impact of COVID-19 pandemic [56,57,58, 63, 64, 67,68,69,70,71,72,73,74,75,76,77,78]. Eight reviews described the role of the pandemic in facilitating a rapid shift towards the increased use of digital health in the background or discussion sections, mostly to justify the need for their review [56, 67, 68, 70,71,72, 74, 75]. Seven reviews mentioned including studies related to the COVID-19 pandemic and factored this into their analysis [57, 64, 69, 73, 76,77,78] to understand things like feasibility of implementation of digital health [64] but did not conduct any analyses related to the impact of digital health on relationships and/or trust. Only two reviews specifically focused on the use of telemental health [58] and remote consultations [63] during the pandemic and reported some positive and negative impacts of these types of technology on patient-provider relationships.
Eight reviews directly examined relationships and/or trust in the context of eHealth [59, 79,80,81,82,83,84,85]. Eleven reviews examined related concepts like communication, interaction, and therapeutic alliance in an eHealth context [61, 62, 86,87,88,89,90,91,92,93,94]. In all other reviews, relationships and/or trust were not the focus but were discussed along with other findings. Tables 2 and 3 outline the characteristics of the included reviews.
Conceptualization of relationships and trust
Patient-provider relationships were defined in six reviews [83, 85, 91, 110, 121, 125]. One review defined trust in doctor-patient relationships [59]. Provider-provider relationships were not defined and only directly referred to in three reviews [53, 54, 107]. These definitions provided some insight into how authors understood and used the terms ‘trust’ and relationships’ within the context of their review. The reviews also used different terms that were either explicitly connected with relationships or were interpreted by us as related to relationships based on our operational definition. Connections between terms were most often not described and challenging to identify (Table 4).
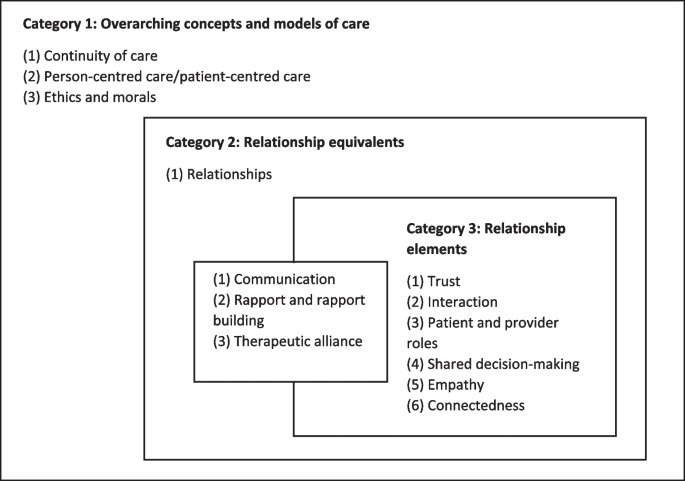
The terms used to refer to patient-provider relationships were organized into three non-mutually exclusive sets: 1) Overarching concepts and care models; 2) Relationship equivalents or elements; and 3) Relationship elements. Overarching concepts and care models (category 1) included terms that encompassed relationships, such as continuity of care, person-centred/patient-centred care, ethics, and morals. Relationship equivalents included terms that were used interchangeably with relationships, whereas relationship elements included terms that were encompassed within relationships. Terms that were both relationship equivalents and elements (category 2) included communication, rapport/rapport-building, and therapeutic alliance. Terms that were only relationship elements (category 3) included trust, interaction, patient and provider roles, shared decision-making, empathy, and connectedness. Some terms that came up less frequently and consistently (e.g., information sharing, support, collaborative care) could not be meaningfully mapped and connected to other concepts. Future research could explore the interpretation and use of these other less frequently used terms. Figure 3 indicates our interpretation of the connections between different terms used for patient-provider relationships.
With respect to provider-provider relationships, we were unable to categorize terms as the smaller number of reviews made it challenging to identify patterns and connections between terms. Terms mostly appeared to be used either interchangeably with relationships or as standalone terms and included: communication, collaboration, interaction, information sharing/exchange, connection, support.
Impact of eHealth on patient-provider relationships
Forty-seven reviews reported a mix of positive and negative impacts of eHealth on patient-provider relationships [16, 54, 57, 59, 62, 64,65,66,67,68, 70, 72, 74, 73, 75, 76, 78,79,80,81, 85, 88, 89, 91, 92, 95,96,97,98,99, 104,105,106,107,108, 112, 113, 116, 117, 120, 122,123,124, 126,127,128,129] (e.g., communicating via technology created a distance between the patient and provider in some instances, but also reduced loneliness in others). Nineteen reviews reported mainly positive impacts (e.g., more collaboration and closeness between patient and provider) [53, 55, 56, 60, 71, 77, 83, 100, 102, 103, 109,110,111, 115, 118, 119, 121, 125, 130] while seven reviews reported mainly negative impacts (e.g., reduced conversation flow) [58, 61, 63, 69, 82, 87, 114]. Three reviews noted no impact of technology on patient-provider relationships [84, 93, 94]. We also noted a collection of factors that influenced whether the impact of eHealth on patient-provider relationships and trust was positive, negative, or neutral. We categorized the influencing factors as patient-related, provider-related, technology-related, and organizational factors. Each category is described below with examples from relevant reviews. Table 5 displays the frequency of factors across different types of technology. Additional file 2 describes the factors and impact reported in each study discussing patient-provider relationships.
Patient-related factors
-
1.
Patient perceptions, expectations, motives, and concernswere the most reported factors influencing relationships and trust (18 reviews), particularly in reviews focusing on management and communication systems. For example, patients had greater trust in providers and satisfaction with the relationship when using Electronic Health Records (EHRs) and telemedicine when they perceived providers as competent, knowledgeable, or experienced [96, 113]. Patient perceptions that remote patient monitoring would replace personal care was related to a negative impact on communication, interaction, and trust, whereas feeling like an “equal partner” when providers included them in discussions about their data was related to a positive impact on relationships [112].
This factor was also discussed in two reviews focusing on information systems. For example, a positive impact on relationships was noted when patients’ motives for seeking online health information were to support rather than challenge the therapeutic relationship [80] and when they were willing to discuss online health information with the provider as compared to when they were afraid of challenging the provider’s authority [85].
-
2.
Patient functional ability was linked to patient-provider relationships in six reviews mostly discussing communication systems. For example, the alliance built through videoconferencing was seen as impaired for patients with epilepsy, post-traumatic stress disorder [62] and cognitive-behavioural challenges [58]. Communication challenges during teleconsultations were reported with patients with visual and hearing impairments [63, 64]. With mental health, the patient-provider relationship was sometimes seen as better (patients were more willing to share information virtually) and sometimes worse (providers perceived a need for human contact to facilitate recovery) when using virtual modalities [54]. One review noted that patients and providers felt that the ability of remote consultations to facilitate patient empowerment and participation could change as the patient’s illness progressed [77].
-
3.
Sociodemographic factors were related to relationships and trust in 10 reviews, mostly focusing on communication systems. With respect to age, remote consultations and telehealth were linked to the development and sustenance of positive and trusting relationships particularly in younger [56] and more computer literate patients [57]. Contrastingly, one review noted that older patients felt that telehealth facilitated discussions with their provider and supplemented standard visits [55].
Three reviews indicated that language barriers can lead to communication systems having a negative impact on patient-provider communication [63,64,65] and one noted that language barriers were more common with patients in high social vulnerability areas [63].
Two reviews indicated that the impact of communication systems like telemental health and mHealth on patient-provider relationships and trust can vary according to socioeconomic status [16, 58]. Two reviews discussing management systems [59] and multiple types of technology [60] reported socioeconomic status as a factor or barrier influencing trust and relationships.
Two reviews discussed the impact of communication and management systems on relationships and trust in minority/disadvantaged groups. One noted a negative impact on relationship-building during telephone consultations for minority patients [57]. The other reported a positive impact on patient trust in providers for disadvantaged patient groups related to the use of Patient Accessible Electronic Health Records (PAEHRs) [66].
Table 6 outlines the varying impact of eHealth by functional ability and sociodemographic factors.
Table 6 Impact of eHealth in different groups -
4.
Familiarity and consistency within the relationship or presence of a pre-existing relationshipwas reported in reviews discussing communication systems (five reviews). For instance, regular and effective patient-provider communication was noted when the provider remained the same [117]. Patients were found to report mostly positive experiences when telehealth facilitated maintenance of a pre-existing relationship [57]. A pre-existing patient-provider relationship when using remote consultations was linked to positive outcomes including enabling providers to engage patients in shared decision-making and self-management [56] and better treatment continuity and clinician outcomes [68]. However, Verma et al. reported that patients found telemedicine impersonal even when they knew their provider [63].
Provider-related factors
-
1.
Providers’ communication skills and technology use style (i.e., provider’s style of using technology during an in-person visit or for remote patient communication) were frequently connected to the impact of technology on relationships and trust (18 reviews), particularly in reviews discussing management and communication systems.
With use of management systems like EHRs during in-person visits, examples of provider behaviours that impacted relationships positively included making computer use less obvious; inviting patients to look at the screen to facilitate conversation particularly during sensitive discussions; maintaining eye contact and conversation with patients [79, 122, 126]; giving patients time to reflect by turning away to enter data on the computer [122]; using technology as a discussion tool for emotional support [69] and collaborative planning and documentation [104]. On the other hand, screen gaze [79, 89, 91, 92], keyboarding [79, 89, 91], closed body posture [79], and indirect facial orientation [91] had a negative impact.
With respect to communication systems (teleconsultations and remote monitoring systems), providers’ ability to develop a “video presence” [65], adjust communication style by using non-verbal cues [62, 65], provide undivided attention and create a supportive and relaxed environment [77], use technology for direct and indirect patient communication [110] and information exchange by sharing charts and test results [113] were linked with a positive impact on relationships.
Nine reviews suggested that the negative impact resulting from the provider’s technology use style and communication can be mitigated by: using strategies specific to the care delivery modality (telephone or video consultation) [58, 64, 77, 124, 129]; provider training in technology use [89, 91], in the limitations and regulations related to technology and in judging appropriateness of the modality [107]; considering the context and patient preferences and experiences while designing and implementing new technologies [89, 72]; and setting clear expectations between patient and provider [81].
-
2.
Provider perceptions, reactions and attitudes were reported in 16 reviews, mostly those discussing communication systems. For example, the impact of mHealth could be positive or negative depending on provider perceptions about the need for face-to-face contact (some wanted in-person contact or expressed concerns with “impersonalization” of interactions), access (some perceived increased access to services through mHealth), and the need for boundary setting (some felt the need to set boundaries to being contactable outside working hours) [16].
Provider perceptions and beliefs were also noted in reviews discussing other types of technology. For example, negative provider perceptions and concerns around the potential for management systems like EHRs to reduce time spent with patients and interfere with direct care provision was linked to a negative impact on relationships [97]. Relating to information systems, a positive impact of patient online health information seeking was noted when providers believed that patients have the right to be informed and created an open environment, whereas a negative impact resulted when providers believed that patients seek online information because they don’t trust them [80].
Differences in impact were also found depending on whether a provider had used technology or not. For instance, providers using management systems (EHRs) and communication systems (remote monitoring equipment and videophone) generally perceived greater positive impact compared to nonusers who anticipated challenges [98, 106]. Two reviews noted that providers’ initial concerns about potential negative impacts of teleconsultations changed to a perceived positive impact after use [75, 77].
In one review, provider perceptions of patient expectations influenced the impact on relationships and trust. For example, providers believed that patients preferred in-person interactions and that use of patient-generated health data would exacerbate social isolation and hinder collaboration [81]. Provider and patient perceptions sometimes conflicted. For example, providers felt that patients found technology difficult to use; however, patients felt that technology reduced anxiety and improved self-management [106].
Technology-related factors
-
1.
Type of care delivery modality (video, phone, or in-person) was the most reported technology-related factor (15 reviews) discussed in reviews of communication systems.
In-person vs. remote (phone and video) consultations
Two reviews found that the therapeutic alliance did not differ for remote and in-person interventions [93, 94] while one found that it was stronger over teleconsultation compared to in-person [68]. Patients and providers reportedly perceived that remote consultations build trust [129], facilitate strong alliances and quick exchanges over time [129], continuity and consistent access to the same provider [56, 129], individualized and timely support [56], leading to positive working relationships [56]. In contrast, one review noted that in-person visits allowed for providing richer information and advice compared to teleconsultations [68] and another reported that increased trust created through asynchronous communication could lead to assumptions about other users’ intentions (e.g., assumption that the other user is being truthful) [129].
One review reported varying perceptions of virtual visits, with some patients and providers noting greater family inclusion and support and others perceiving less compassion, empathy, and discomfort with the possibility of multiple people watching during video visits [78]. Another noted that providers perceived blended care (mix of in-person and remote care) as “different” but “not necessarily worse” than in-person care; some providers were surprised by their ability to build relationships online and found that blended models provided more opportunities for rapport, support, and monitoring [128].
In-person vs. phone consultations
The alliance over phone consultations was found to be “different” compared to in-person care in one review focused on psychological therapy; greater task/treatment focus over the phone appeared to compensate for a reduction in bond, made it easier to stick to time boundaries, and, in one review, patients found the visual anonymity beneficial [88].
In-person vs. video consultations
Compared to in-person consultations, relationship-building over videoconferencing took longer and resulted in reduced conversation flow [111]. The therapeutic alliance could either be equivalent, improved, or impaired in videoconferencing compared to in-person depending on the patient’s diagnosis and the therapist’s and patient’s ability to adjust communication styles [62]. Providers found that videoconferencing provided more time to deliver personalized care and patients perceived more individual attention and focus via videoconferencing compared to in-person consultations after initial scepticism [76]. Videoconferencing was also reported to lead to loss of professional boundaries when patients were unintentionally able to view providers’ homes, leading to patients getting more personal information than the provider would like [58].
Phone vs. video consultations
Compared to phone consultations, patients and providers perceived that videoconferencing increased closeness, engagement, and continuity [111], facilitated rapport building [68] and non-verbal communication [57]. Phone consultations reportedly limited capacity for relationship-building and maintaining therapeutic alliance due to limited access to non-verbal cues [57, 58, 68, 78], particularly among minority participants [57]. Some patients desired to see the provider’s reaction and perceived inadequate time for questions during audio-only visits as compared to video and in-person consultations [78]. However, some also valued the “undivided communication” offered via phone-based interventions [74]. One review noted that patients reported more positive experiences with both phone and video consultations being used together [57].
-
2.
Technology design and featureswere reported in 10 reviews, across management, communication, and information systems. For example, personalized design, real-time monitoring, and two-way communication through mHealth apps were reported to improve information sharing and continuity of care, facilitate power and responsibility sharing, and increase trust [83]. Features like provider access to trends and summary measures [81], joint viewing of imaging results with patients [90], screensharing and document editing [56], and integration of social determinants of health [60] in EHRs and Patient Generated Health Data (PGHD) supported collaboration, communication, and shared decision-making. Technology that provided opportunities for communication was perceived by patients to reduce isolation, increase trust in the provider, and led to providers perceiving patients to be “more open”, whereas technology that reduced communication led to patients missing human contact and created a “distance” [67]. One review identified usability (e.g., ease of use) as important for synchronous technology like video consults and asynchronous remote decision-making technology to facilitate partnerships and interactions [71].
Organizational factors
Organizational factors relating to implementation and use of technology were reported in three reviews that discussed multiple types of technology. For example, implementers were noted to be concerned about the potential negative impact of technology like Electronic Medical Records (EMRs), EHRs, and computerized clinical decision support systems on patient-provider relationships [122]. The absence of guidelines and insufficient training for using technology were reported as impediments, and stakeholder engagement as an enabler of stakeholder trust in technology [59]. Synchronous technology like video consults and asynchronous shared decision-making technology could reportedly facilitate “partnerships” and “remote interactions” if factors like training in technology use and broadband access were addressed [71].
Impact of eHealth on provider-provider relationships
eHealth appeared to have a positive (7 reviews) [53, 55, 98, 102, 111, 113, 114], negative (6 reviews) [58, 64, 73, 86, 97, 101], or mixed (9 reviews) [16, 54, 67, 77, 87, 90, 99, 107, 108] impact on provider-provider relationships depending on provider-related, technology-related, and organizational factors. Examples from relevant reviews describing each category of factors are discussed in this section. Table 7 displays the frequency of each factor across types of technology. Additional file 3 describes the factors and impact reported in each study discussing provider-provider relationships.
Provider-related factors
-
1.
Provider communication and technology use skills/style were reported to influence provider-provider relationships in four reviews discussing management and communication systems. With respect to communication systems, a negative impact was noted when providers had impaired technical communication skills like sending delayed email responses (potentially leading to friction) and because of limited non-verbal cues and informal contact in virtual teams (leading to weaker working relationships) [107]. On the other hand, clarification actions (or “utterances” intended to clarify and understand) between providers while using videoconferencing equipment were reported to enhance collaborative working [87].
For management systems, providers with higher skill in technology use perceived greater benefit from EMRs [98]. Providers’ technology use style (e.g., frequent use of the copy-and-paste function) led to “cluttered” notes and limited providers’ ability to develop “shared understandings” [101].
-
2.
Provider attitudes towards and perceptions of technology were noted to impact team relationships in two reviews (one discussing mana>gement systems and the other discussing multiple technologies). For example, negative provider perceptions of EMR as “management control systems” were reported to infringe on privacy and autonomy [97]. Providers’ lack of willingness to learn how to use online communities was reported to be a barrier to the otherwise positive impact of the technology on interprofessional collaboration [86].
Technology-related factors
-
1.
Technology features and design were linked to a negative impact on team relationships in three reviews (one discussing management systems, one discussing communication systems and the other discussing multiple types of technology). Relating to management systems, the templated structure of EHR, lack of ease in informational retrieval, lack of representational structures for communicating nurse, patient, and psychosocial perspectives on care had a negative impact on team communication [101]. With communication systems, unidirectional paging systems were noted to impair communication [90]. One review discussing multiple types of technology reported positive or negative provider perceptions of team communication and teamwork depending on the ability of the technology to connect members (e.g., when technology did not have features that allowed physicians to connect with specialists, it negatively impacted communication) [67].
-
2.
Fit between task and technology was reported in one review discussing multiple types of technology; selecting communication technology that fits the task was found necessary to support team routines and communication [107].
Organizational factors
Availability of resources like standards and guidelines, training, strategic and creative adaptations was reported to be vital for facilitating virtual team operations and dynamics [107]. The extent of perceived benefit of EMR was linked to the size of the practice, such that larger practices saw greater benefit of EMR in communicating with other providers and organizations.
Discussion
This review of reviews intended to better understand how eHealth impacts patient-provider and provider-provider relationships and trust in primary care by examining existing evidence syntheses. We found 79 reviews that described the impact of management systems, communication systems, information systems, and computerized decision support systems on relationships and trust. Most of the reviews discussed patient-provider relationships and only a small number focused on provider-provider relationships. Overall, management and communication systems were the most frequently discussed types of eHealth technologies and they appeared to have a mixed impact (both positive and negative) on patient-provider and provider-provider relationships and trust.
A steady increase was observed in the number of reviews emerging in this area, particularly in 2021 and 2022. However, only a few intentionally examined and clearly defined relationships and trust. Most of the included reviews had explored the impact of eHealth on relationships as part of another primary aim. Therefore, this impact and the influencing factors were not always explicitly or directly described. This made it challenging to understand what impact the use of technology was having on relationships and why, and often called for us to make connections based on our interpretations. The fluid and expanding nature of eHealth as a group of technologies [14] further adds to the complexity of this issue. For the sake of convenience, we limited our analysis to the four types of eHealth technologies within Mair et al.’s classification [15].
The terms ‘relationships’ and ‘trust’ were not defined in most of the included reviews and several interrelated terms such as ‘communication’ and ‘information-sharing’ were used without drawing out clear connections between each other. Often there appeared to be an underlying assumption that the reader would share the same implicit definition as the authors. Additionally, limited reporting of the authors’ epistemological background made it difficult to unpack these concepts in a meaningful manner. This resulted in a definitional soup or lack of conceptual clarity on what ‘relationships’ and ‘trust’ mean within the context of a specific review. Our analytical challenges in disentangling and interpreting the various terms used made it difficult to determine the impact of eHealth on the different elements or aspects of relationships. This finding points towards the need for better taxonomies in this area that conceptualise relationships, trust, and interrelated terms within the context of eHealth. The conceptualisation we have proposed in this review (Fig. 3) could serve as a starting point that could be built on using participatory approaches with experts (e.g., patients, caregivers, providers, managers) such as Delphi or deliberative methods [131].
Our analysis revealed a mixed impact of eHealth on patient-provider relationships and trust. This impact appeared to be positive, negative, or mixed depending on different influencing factors (patient-, provider-, technology-related, and organizational factors or a combination of these). These influencing factors were not always mentioned directly (if mentioned at all) in the included reviews and were often difficult to identify, possibly indicating the need for more work that is directly focused on understanding how these human and non-human factors might be impacting relationships and trust while using technology.
Of the patient-related factors, ‘patient perceptions, expectations, motives, and concerns’ were most frequently found to influence the impact of management and communication systems on patient-provider relationships. Patients often seemed to perceive a positive impact of these types of technology on the relationship when they perceived that it supported personalised and collaborative care. Another patient- and provider-related factor that came up in more recent reviews (from 2021 onwards) and was associated with a positive impact on the patient-provider relationship was familiarity or presence of a pre-established relationshipprior to using communication systems like telehealth. These findings suggest that these types of technology are more likely to positively impact relationships and trust when used as part of hybrid care delivery models (where virtual care is used to support patient-provider relationships that have been established through initial in-person interactions) rather than a “digital-first” approach [13]. Similar recommendations have been provided in recent reports and policy documents to guide the use of technology in primary care delivery. For instance, the 2022 Virtual Care Task Force Report in Canada notes that this type of care may be better used “in the context of an ongoing relationship with a family physician or specialist and their care team” ([10] p17). Likewise, the American College of Physicians Policy Recommendations on telemedicine recommend that it “can be most efficient and beneficial between a patient and physician with an established ongoing relationship” ([132] p788).
Our analysis found a small number of reviews that discussed the impact of eHealth on patient-provider relationships (and none on provider-provider relationships) using an equity lens. Equity and the differential impact of technology among different groups on relationships was not considered as a primary aim of most reviews and usually reported as part of other findings, suggesting a need for a more explicit focus on this aspect in future studies. We found a possible differential impact of communication systems (and less frequently of management systems) on patient-provider relationships based on certain sociodemographic factors. eHealth mostly appeared to positively impact patient-provider relationships among younger patients, but there was some evidence that this positive impact could extend to older patients as well. These findings are similar to Rodgers et al.’s review [50] that found that although younger healthier patients tend to use digital consultations more, some older patients do use it as well. The impact of eHealth was also linked to the patient’s functional abilities and/or health condition. When there were language barriers between patients and providers and for patients with visual, auditory, and cognitive-behavioural challenges, eHealth appeared to negatively impact relationship. In the case of mental health conditions, a varied impact was reported. Therefore, eHealth needs to be used judiciously in these situations, possibly by identifying ways to work through challenges that may arise while working with some patients (for example, by offering patients a choice between virtual and in-person consultations, using virtual consultations as a supplement to in-person care only when preferred or needed, designing technology that better fits individual patients’ needs). Overall, these findings indicate that it is important for providers and organizations to be mindful of these sociodemographic factors and patient preferences in order to facilitate relationship building and maintenance when implementing eHealth solutions. Providers and organizations also need to consider existing inequities in terms of digital literacy and patient access to technology and internet connectivity to ensure that the use of eHealth does not exacerbate existing healthcare disparities [133]. Designing and adapting technology that meets the needs of different patient groups can also ensure that the positive impacts of technology on building relationships and trust with these groups are not lost.
Among the provider-related factors, ‘provider communication skills and technology use style’(in relation to management and communication systems) were the most frequently reported, particularly during teleconsultations as well as relating to the use of EHRs during in-person consultations. When providers were able to successfully use technology-specific communication skills (like effective non-verbal communication during remote consultations and while accessing EHRs during in-person consultations), there was a positive impact on relationships and trust. While there is already evidence to suggest that provider communication and interaction styles can influence the therapeutic alliance [134], our findings add to this by highlighting the need for providers to adapt these communication skills to the type of technology being used in order to effectively build relationships with patients. While previous research has highlighted the need to train providers in communication and technology use [49], our review specifically brings out the possible benefits of training on optimizing the positive impact of technology on the patient-provider relationship and trust, and how this training may need to account for patient characteristics and needs, technology functionality and organizational contexts. Initiating training early on during medical school and offering continued opportunities for training during post graduate education and through continuing professional development can help providers build skills in using and communicating via technology.
‘Provider perceptions, attitudes, and concerns’(in relation to communication systems) were also frequently found to influence the impact of eHealth on patient-provider relationships and trust. Although negative provider perceptions about technology sometimes seemed to have a negative impact on the patient-provider relationship [80, 97], we found that these perceptions could change after providers use technology (see for example Walthall et al., [77] Bassi et al., [98] Brewster et al., [106] and Sharma et al. [75]). We also found that there were some discrepancies between providers’ perceptions of patient expectations and patients’ actual expectations regarding technology use (see for example Brewster et al. [106]). These findings could be because included reviews sometimes appeared to report providers’ perceptions of technology based on its anticipated rather than experienced impact on relationships and trust. It was often challenging to distinguish which of the two the review focused on and making this distinction may have helped us analyse the findings better. More research that collects patients’ and providers’ actual experiences of using technology and its impact on their relationships could help better understand the experienced rather than perceived impact. As well, mutual clarification of expectations regarding use of technology between patients and providers can help optimize its positive impact on their relationship with each other.
With respect to technology-related factors, the type of care delivery modality was most frequently found to influence the impact of communication systems on patient-provider relationships. We found mixed evidence on the impact of different types of care delivery modalities (phone, video and in-person consultations). While describing the impact of communication systems on relationships, some reviews did not distinguish between telephone and video consultations when referring to virtual care (see for example, Keenan et al. [72]). As a result, it was difficult to determine which care delivery modality had positive or negative impacts and when. Technology design and features were also found to influence the impact of management, communication, and information systems on patient-provider relationships, with a more positive impact noted with technology that facilitated collaboration and communication. These technology-related factors were often reported along with patient- and provider-related factors. For example, what was considered an appropriate care delivery modality depended on patient and provider perceptions (such as in Penny et al. [111] where providers perceived that videoconferencing prolonged the relationship-building process compared to in-person consultations). This suggests that considering these technology-related factors together with person-related factors and targeting the modifiable factors (e.g., increasing awareness and education to change patient and provider perceptions and attitudes towards technology, training providers in communication skills, and designing and choosing technology that meets patient needs) can help achieve good technology-person fit to help facilitate positive patient-provider relationships. Notably, some common technology-related measures like satisfaction were not represented in these reviews, suggesting a potential gap in understanding how usability measures like satisfaction may play a role in patient-provider and provider-provider relationships [135].
Given the very small number of reviews that discussed the impact of eHealth on provider-provider relationships, we were unable to clearly determine the impact by the type of technology. However, the influencing factors that our analysis identified were similar to those influencing the impact of patient-provider relationships. Impaired provider communication and technology use style (such as poor email communication skills and ineffective use of EMR functions), negative provider perceptions of technology, unwillingness of providers to learn about technology, and technology design that did not facilitate communication or ease of use were linked with a negative impact on provider-provider relationships. Organizations can potentially address these factors through strategies such as encouraging initial in-person communication and frequent and continuous communication between providers [136], improving providers’ knowledge of and motivation to use technology [136], and choosing technology that fits with team members and the situation [137]. As teams increasingly work in hybrid environments, organizational behaviour literature can provide valuable insights into optimal ways in which teams can build relationships [138].
Although some of the reviews included in our study provided a few recommendations for the use of technology in primary care settings, these were not always clearly stated or presented as actionable strategies, nor did they directly focus on relationships or trust. Our review addresses this gap by presenting some key recommendations and implications for different stakeholders (such as patients, providers, managers, policy makers, educators, and technology developers) relating to optimal ways to design and use eHealth to facilitate relationship and trust building in different aspects of primary care (such as care delivery, care coordination, team communication, and training/education). These recommendations have been proposed based on the authors’ analysis of the findings from the included reviews and are outlined in Table 8.
Strengths and limitations
By focusing on the relational aspects of primary care in the context of eHealth technologies, this review of reviews addresses an important issue, particularly in the current post-pandemic context where primary care settings are increasingly contemplating how best to integrate technology into care delivery. The recommendations offered for different stakeholders within primary care can inform decision-making around when and how to use different types of eHealth technologies. The search strategy for this review was rigorously developed and implemented. Although single reviewer screening may have led to some relevant articles being excluded, we attempted to minimize this by conducting multiple rounds of agreement checks and discussions between team members to ensure consistency during screening and data extraction. A quality appraisal of each included review was not indicated as this review aimed to provide an overview of existing knowledge in the area [139]. This may have also contributed to our including a wide range of literature thereby providing a comprehensive synthesis of the evidence in this area. The findings of this review also need to be considered in light of certain limitations. Firstly, as relationships and trust were discussed using several interrelated terms that were not always clearly defined, our analysis and findings are based on our interpretation of these terms. We acknowledge that these terms could be interpreted in multiple ways and that the authors of the included reviews may have their own interpretations. The conceptualization presented in this paper represents one way of interpreting these terms. This variation in terminology used and interpretations could have also led to some relevant articles being excluded.
As this study focused on reviews rather than studies discussing individual technologies, the type of technology discussed in different reviews had to be abstracted to high-level categories using an existing classification system (communication, management, information, and computerized decision support systems). As a result, it was difficult to determine the type of impact (positive, negative, or neutral) of individual technologies. Most of the included reviews discussed communication and management systems. As very few reviews discussed computerized decision support systems and information systems or discussed these along with other types of eHealth technologies, it was hard to draw meaningful conclusions about these two types of technologies. While beyond the scope of our study, we do recognize that patient and provider relationships in primary care settings may be influenced by access to and care delivery from other care providers and specialists which is not captured in our results. The findings presented are mostly reflective of the impact of communication and management systems on relationships and trust in primary care settings and should be considered within this context.
Conclusion
eHealth impacts relationships and trust in positive and negative ways depending on how it is used and who is using it. The potential positive impacts can be lost if it is not used effectively, and negative impacts can be mitigated or compensated for through different strategies, such as designing and using technology that meets the needs of the situation and people involved, and training providers in using and communicating appropriately with technology. The findings of this review have implications for healthcare providers, patients, managers, educators, policy makers, technology developers, and other stakeholders’ decision-making around optimal ways to integrate eHealth in primary care to facilitate relationship-building and maintenance.
Availability of data and materials
Data generated and analysed during this study are largely included in this published article (and its supplementary information files). Raw data sets used to initially collect and sort data can be made available upon request.
References
Starfield B. Primary care: an increasingly important contributor to effectiveness, equity, and efficiency of health services. SESPAS report 2012. Gac Sanit. 2012;26:20–6. https://doi.org/10.1016/j.gaceta.2011.10.009.
Thomas-MacLean R, Tarlier D, Fortin M, Ackroyd-Stolarz S, Stewart M. TUTOR-PHC 2003/2004 research trainees “no cookie-cutter response” conceptualizing primary health care. 2008. https://www.uwo.ca/fammed/csfm/tutor-phc/training/trainingmanuals.html. Accessed 28 Jan 2023.
Suter E, Mallinson S, Misfeldt R, Boakye O, Nasmith L, Wong ST. Advancing team-based primary health care: a comparative analysis of policies in western Canada. BMC Health Serv Res. 2017;17(1):493. https://doi.org/10.1186/s12913-017-2439-1.
Russell GM, Miller WL, Gunn JM, Levesque JF, Harris MF, Hogg WE, Scott CM, Advocat JR, Halma L, Chase SM, Crabtree BF. Contextual levers for team-based primary care: lessons from reform interventions in five jurisdictions in three countries. Fam Pract. 2018;35(3):276–84. https://doi.org/10.1093/fampra/cmx095.
Wagner EH, Flinter M, Hsu C, Cromp D, Austin BT, Etz R, Crabtree BF, Ladden MD. Effective team-based primary care: observations from innovative practices. BMC Fam Pract. 2017;18(1):13. https://doi.org/10.1186/s12875-017-0590-8.
Ontario Ministry of Health and Ministry of Long-Term Care: Primary care payment models in Ontario. 2020. https://health.gov.on.ca/en/pro/programs/pcpm/. Accessed 28 Jan 2023.
Schuttner L, Parchman M. Team-based primary care for the multimorbid patient: Matching complexity with complexity. Am J Med. 2019;132(4):404–6. https://doi.org/10.1016/j.amjmed.2018.09.029.
World Health Organization. Global strategy on digital health 2020–2025. 2021. https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf. Accessed 23 Jan 2023.
European Commission. Communication from the Commission to the European Parliament, the European Council, the Council, the European Economic and Social Committee and the Committee of the Regions on enabling the digital transformation of health and care in the Digital Single Market; empowering citizens and building a healthier society. 2018. https://digital-strategy.ec.europa.eu/en/library/communication-enabling-digital-transformation-health-and-care-digital-single-market-empowering. Accessed 23 Jan 2023.
Canadian Medical Association and The College of Family Physicians of Canada. Virtual care in Canada: Progress and potential. Report of the Virtual Care Task Force. 2022. https://www.cma.ca/sites/default/files/2022-02/Virtual-Care-in-Canada-Progress-and-Potential-EN.pdf Accessed 23 Jan 2023.
Omboni S, Padwal RS, Alessa T, Benczúr B, Green BB, Hubbard I, Kario K, Khan NA, Konradi A, Logan AG, Lu Y, Mars M, McManus RJ, Melville S, Neumann CL, Parati G, Renna NF, Ryvlin P, Saner H, Schutte AE, Wang J. The worldwide impact of telemedicine during COVID-19: current evidence and recommendations for the future. Connect Health. 2022;1:7–35. https://doi.org/10.20517/ch.2021.03.
Canadian Institute for Health Information (CIHI). Increase in virtual care services provided by physicians. 2021. https://www.cihi.ca/en/health-workforce-in-canada-highlights-of-the-impact-of-covid-19/increase-in-virtual-care-services. Accessed 23 Jan 2023.
Donnelly T. Digital first primary care and how the NHS Long Term Plan set a clear direction to mainstream digitally enabled care across the NHS. 2020. https://www.england.nhs.uk/blog/digital-first-primary-care-and-how-the-nhs-long-term-plan-set-a-clear-direction/. Accessed 10 October 2021.
World Health Organization. WHO guideline: Recommendations on digital interventions for health system strengthening. 2019. https://www.who.int/publications/i/item/9789241550505 Accessed 23 Jan 2023.
Mair F, May C, Murray E, Finch T, Anderson G, O’Donnell C, Wallace P, Epstein O. Understanding the implementation and integration of e-health services. J Telemed Telecare. 2007;13(1):36–7. https://doi.org/10.1258/135763307781645112.
Odendaal WA, Watkins JA, Leon N, Goudge J, Griffiths F, Tomlinson M, Daniels K. Health workers’ perceptions and experiences of using mHealth technologies to deliver primary healthcare services: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;3(3):CD011942. https://doi.org/10.1002/14651858.CD011942.pub2.
Bova C, Route PS, Fennie K, Ettinger W, Manchester GW, Weinstein B. Measuring patient-provider trust in a primary care population: Refinement of the Health Care Relationship Trust scale et al.,. Res Nurs Health. 2012;35(4):397–408.
Pagliari C. Digital health and primary care: Past, pandemic and prospects. J Glob Health. 2021;11:01005. https://doi.org/10.7189/jogh.11.01005.
Song H, Ryan M, Tendulkar S, Fisher J, Martin J, Peters AS, Frolkis J, Rosenthal MB, Chien AT, Singer SJ. Team dynamics, clinical work satisfaction, and patient care coordination between primary care providers: A mixed methods study. Health Care Manage Rev. 2017;42(1):28–41. https://doi.org/10.1097/HMR.0000000000000091.
Xyrichis A, Lowton K. What fosters or prevents interprofessional teamworking in primary and community care? A literature review. Int J Nurs Stud. 2008;45(1):140–53. https://doi.org/10.1016/j.ijnurstu.2007.01.015.
Cole MB, McLean V. Therapeutic relationships re-defined. Occup Ther Ment Health. 2003;19(2):33–56. https://doi.org/10.1300/J004v19n02_03.
Phillips-Salimi CR, Haase JE, Kooken WC. Connectedness in the context of patient-provider relationships: A concept analysis. J Adv Nurs. 2012;68(1):230–45. https://doi.org/10.1111/j.1365-2648.2011.05763.x.
Gelso C. A tripartite model of the therapeutic relationship: Theory, research, and practice. Psychother Res. 2014;24(2):117–31. https://doi.org/10.1080/10503307.2013.845920.
Miciak M, Mayan M, Brown C, Joyce AS, Gross DP. The necessary conditions of engagement for the therapeutic relationship in physiotherapy: An interpretive description study. Arch Physiother. 2018;8(3):1–12. https://doi.org/10.1186/s40945-018-0044-1.
Lanham HJ, McDaniel RR Jr, Crabtree BF, Miller WL, Stange KC, Talia AF, Nutting PA. How improving practice relationships among clinicians and nonclinicians can improve quality in primary care. Jt Comm J Qual Patient Saf. 2009;35(9):457–66. https://doi.org/10.1016/S1553-7250(09)35064-3.
Lee CT, Doran DM. The role of interpersonal relations in healthcare team communication and patient safety: A proposed model of interpersonal process in teamwork. Can J Nurs Res. 2017;49(2):75–93. https://doi.org/10.1177/0844562117699349.
Raj M, Wilk AS, Platt JE. Dynamics of physicians’ trust in fellow health care providers and the role of health information technology. Med Care Res Rev. 2021;78(4):338–49. https://doi.org/10.1177/1077558719892349.
Robinson CA. Trust, health care relationships, and chronic illness: A theoretical coalescence. Glob Qual Nurs Res. 2016;3:1–11. https://doi.org/10.1177/2333393616664823.
Tarrant C, Dixon-Woods M, Colman AM, Stokes T. Continuity and trust in primary care: A qualitative study informed by game theory. Ann Fam Med. 2010;8(5):440–6. https://doi.org/10.1370/afm.1160.
Murray B, McCrone S. An integrative review of promoting trust in the patient-primary care provider relationship. J Adv Nurs. 2015;71(1):3–23. https://doi.org/10.1111/jan.12502.
Chipidza FE, Wallwork RS, Stern TA. Impact of the doctor-patient relationship. Prim Care Companion CNS Disord. 2015;17(5):1–24. https://doi.org/10.4088/PCC.15f01840.
Chen W, Feng Y, Fang J, Wu J, Huang X, Wang X, Wu J, Zhang M. Effects of trust in primary care physicians on patient satisfaction: A cross-sectional study among patients with hypertension in rural China. BMC Fam Pract. 2020;21(1):1–13. https://doi.org/10.1186/s12875-020-01268-w.
Thom DH, Hall MA, Pawlson LG. Measuring patients’ trust in physicians when assessing quality of care. Health Aff (Millwood). 2004;23(4):124–32. https://doi.org/10.1377/hlthaff.23.4.124.
College of Physicians and Surgeons of Ontario and Citizen Advisory Group. Continuity of care. Guide for patients and caregivers. https://www.cpso.on.ca/admin/CPSO/media/Documents/public/public-information/coc-guide/coc-guide-patients-caregivers.pdf. Accessed 23 Jan 2023.
Henson P, Wisniewski H, Hollis C, Keshavan M, Torous J. Digital mental health apps and the therapeutic alliance: initial review. BJPsych Open. 2019;5(e15):1–5. https://doi.org/10.1192/bjo.2018.86.
Mesko B, Győrffy Z. The rise of the empowered physician in the digital health era: Viewpoint. J Med Internet Res. 2019;21(3):1–8. https://doi.org/10.2196/12490.
Luk CY. The impact of digital health on traditional health care system and doctor-patient relationship: The case study of Singapore. In: Manoharan AP, McQuiston J, editors. Innovative perspectives on public administration in the digital age. Hershey, PA: IGI Global; 2018. p. 143–67.
Ho A, Quick O. Leaving patients to their own devices? Smart technology, safety and therapeutic relationships. BMC Med Ethics. 2018;19(1):1–6. https://doi.org/10.1186/s12910-018-0255-8.
Segar J, Rogers A, Salisbury C, Thomas C. Roles and identities in transition: Boundaries of work and interprofessional relationships at the interface between telehealth and primary care. Health Soc Care Community. 2013;21(6):606–13. https://doi.org/10.1111/hsc.12047.
Cavanagh K, Millings A. (Inter)personal computing: The role of the therapeutic relationship in E-mental health. J Contemp Psychother. 2013;43:197–206. https://doi.org/10.1007/s10879-013-9242-z.
Misra AJ, Ong SY, Gokhale A, Khan S, Melnick ER. Opportunities for addressing gaps in primary care shared decision-making with technology: a mixed-methods needs assessment. JAMIA Open. 2019;2(4):447–55. https://doi.org/10.1093/jamiaopen/ooz027.
Kozikowski A, Shotwell J, Wool E, Slaboda JC, Abrashkin KA, Rhodes K, Smith KL, Pekmezaris R, Norman GJ. Care team perspectives and acceptance of telehealth in scaling a home-based primary care program: Qualitative study. JMIR Aging. 2019;2(1):1–9. https://doi.org/10.2196/12415.
Maunder R, Chaukos D, Lawson A. Healthcare workers as recipients of compassion: Resilience, burnout, and relationship. In: Hodges BD, Paech G, Bennett J, editors. Without compassion, there is no healthcare. Quebec, CA: McGill-Queen’s University Press; 2020. p. 105–24.
Graves M, Doucet S. Factors affecting interprofessional collaboration when communicating through the use of information and communication technologies: A literature review. J Res Interprof Pract Educ. 2016;6(2):1–33. https://doi.org/10.22230/jripe.2017v6n2a234.
Paul DL, McDaniel RR Jr. A field study of the effect of interpersonal trust on virtual collaborative relationship performance. MIS Q. 2004;28(2):183–227. https://doi.org/10.2307/25148633.
Boers SN, Jongsma KR, Lucivero F, Aardoom J, Büchner FL, de Vries M, Honkoop P, Houwink EJF, Kasteleyn MJ, Meijer E, Pinnock H, Teichert M, van der Boog P, van Luenen S, van der Kleij RMJJ, Chavannes NH. SERIES: eHealth in primary care. Part 2: Exploring the ethical implications of its application in primary care practice. Eur J Gen Pract. 2020;26(1):26–32. https://doi.org/10.1080/13814788.2019.1678958.
Aromataris E, Fernandez R, Godfrey C, Holly C, Khalil H, Tungpunkom P. Methodology for JBI umbrella reviews. In: Joanna Briggs Institute Reviewers’ Manual. 2014. https://ro.uow.edu.au/smhpapers/3344/. Accessed 5 Oct 2021.
Anaya YB, Mota AB, Hernandez GD, Osorio A, Hayes-Bautista DE. Post-pandemic telehealth policy for primary care: an equity perspective. J Am Board Fam Med. 2022;35(3):588–92. https://doi.org/10.3122/jabfm.2022.03.210509.
de Grood C, Raissi A, Kwon Y, Santana MJ. Adoption of e-health technology by physicians: a scoping review. J Multidiscip Healthc. 2016;9:335–44. https://doi.org/10.2147/JMDH.S103881.
Rodgers M, Raine G, Thomas S, Harden M, Eastwood A. Informing NHS policy in ‘digital-first primary care’: a rapid evidence synthesis. Health Serv Deliv Res. 2019;7(41):1–154. https://doi.org/10.3310/hsdr07410.
Belur J, Tomspon L, Thornton A, Simon M. Interrater reliability in systematic review methodology: Exploring variation in coder decision-making. Sociol Methods Res. 2018;50(2):837–65. https://doi.org/10.1177/0049124118799372.
Viera AJ, Garret JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37(5):360–3.
Rouleau G, Gagnon M, Côté J, Payne-Gagnon J, Hudson E, Dubois C. Impact of information and communication technologies on nursing care: Results of an overview of systematic reviews. J Med Internet Res. 2017;19(4):1–21. https://doi.org/10.2196/jmir.6686.
LeBlanc M, Petrie S, Paskaran S, Carson DB, Peters PA. Patient and provider perspectives on eHealth interventions in Canada and Australia: a scoping review. Rural Remote Health. 2020;20(3):5754. https://doi.org/10.22605/RRH5754.
Drovandi A, Wong S, Seng L, Crowley B, Alahakoon C, Banwait J, Fernando ME, Golledge J. Remotely delivered monitoring and management of diabetes-related foot disease: an overview of systematic reviews. J Diabetes Sci Technol. 2023;17(1):59–69. https://doi.org/10.1177/19322968211012456.
Kinley E, Skene I, Steed E, Pinnock H, McClatchey K. Delivery of supported self-management in remote asthma reviews: A systematic rapid realist review. Health Expect. 2022;25(4):1200–14. https://doi.org/10.1111/hex.13441.
Spelten ER, Hardman RN, Pike KE, Yuen EYN, Wilson C. Best practice in the implementation of telehealth-based supportive cancer care: Using research evidence and discipline-based guidance. Patient Educ Couns. 2021;104(11):2682–99. https://doi.org/10.1016/j.pec.2021.04.006.
Siegel S, Zuo Y, Moghaddamcharkari N, McIntyre RS, Rosenblat JD. Barriers, benefits and interventions for improving the delivery of telemental health services during the coronavirus disease 2019 pandemic: a systematic review. Curr Opin Psychiatry. 2021;34(4):434–43. https://doi.org/10.1097/YCO.0000000000000714.
Adjekum A, Blasimme A, Vayena E. Elements of trust in digital health systems: scoping review. J Med Internet Res. 2018;20(12):1–10. https://doi.org/10.2196/11254.
Wark K, Cheung K, Wolter E, Avey JP. “Engaging stakeholders in integrating social determinants of health into electronic health records: a scoping review. Int J Circumpolar Health. 2021;80(1):1–12. https://doi.org/10.1080/22423982.2021.1943983.
Barbosa IDA, da Silva KCDCD, da Silva VA, da Silva MJP. The communication process in telenursing: integrative review. Rev Bras Enferm. 2016;69(4):765–72. https://doi.org/10.1590/0034-7167.2016690421i.
Simpson SG, Reid CL. Therapeutic alliance in videoconferencing psychotherapy: A review. Aus J Rural Health. 2014;22(6):280–99. https://doi.org/10.1111/ajr.12149.
Verma P, Kerrison R. Patients’ and physicians’ experiences with remote consultations in primary care during the COVID-19 pandemic: a multi-method rapid review of the literature. BJGP Open. 2022;6(2):1–16. https://doi.org/10.3399/BJGPO.2021.0192.
Lindenfeld Z, Berry C, Albert S, Massar R, Shelley D, Kwok L, Fennelly K, Chang JE. Synchronous home-based telemedicine for primary care: a review. Med Care Res Rev. 2022;1–13. https://doi.org/10.1177/10775587221093043.
Henry BW, Block DE, Ciesla JR, McGowan BA, Vozenilek JA. Clinician behaviors in telehealth care delivery: a systematic review. Adv in Health Sci Educ. 2017;22(4):869–88. https://doi.org/10.1007/s10459-016-9717-2.
Benjamins J, Haveman-Nies A, Gunnink M, Goudkuil A, de Vet E. How the use of a Patient-Accessible Health Record contributes to patient-centered care: Scoping review. J Med Internet Res. 2021;23(1):1–14. https://doi.org/10.2196/17655.
Al-Naher A, Downing J, Scott KA, Pirmohamed M. Factors affecting patient and physician engagement in remote health care for heart failure: Systematic review. JMIR Cardio. 2022;6(1):1–13. https://doi.org/10.2196/33366.
de Albornoz SC, Sia K, Harris A. The effectiveness of teleconsultations in primary care: Systematic review. Fam Pract. 2022;39(1):168–82. https://doi.org/10.1093/fampra/cmab077.
Diaz MF, Colleen G, Gruver R, Gold MA, Maier M, Usseglio J, Garbers S. Providing contraceptive health services to adolescents and young adults by telemedicine: a scoping review of patient and provider perspectives. J Pediatr Adolesc Gynecol. 2022;35(5):575–84. https://doi.org/10.1016/j.jpag.2022.05.003.
Gorrie A, Gold J, Cameron C, Krause M, Kincaid H. Benefits and limitations of telegenetics: a literature review. J Genet Couns. 2021;30(4):924–37. https://doi.org/10.1002/jgc4.1418.
Hartasanchez SA, Heen AF, Kunneman M, García-Bautista A, Hargraves IG, Prokop LJ, May CR, Montori VM. Patient Educ Couns. 2022;105(2):356–65. https://doi.org/10.1016/j.pec.2021.06.012.
Keenan AJ, Tsourtos G, Tieman J. The value of applying ethical principles in telehealth practices: systematic review. J Med Internet Res. 2021;23(3):1–10. https://doi.org/10.2196/25698.
Lampickiene I, Davoody N. Healthcare professionals’ experience of performing digital care visits – A scoping review. Life (Basel). 2022;12(6):1–22. https://doi.org/10.3390/life12060913.
Shah N, Costello K, Mehta A, Kumar D. Applications of digital health technologies in knee osteoarthritis: Narrative review. JMIR Rehabil Assist Technol. 2022;9(2):1–30. https://doi.org/10.2196/33489.
Sharma G, Devan K. The effectiveness of telepsychiatry: thematic review. BJPsych Bull. 2021;1–8. https://doi.org/10.1192/bjb.2021.115.
Wallace LM, Falla D, Rushton A, Heneghan NR. Group and individual telehealth for chronic musculoskeletal pain: a scoping review. Musculoskeletal Care. 2022;20(2):245–58. https://doi.org/10.1002/msc.1594.
Walthall H, Schutz S, Snowball J, Vagner R, Fernandez N, Bartram N. Patients’ and clinicians’ experiences of remote consultation? A narrative synthesis. J Adv Nurs. 2022;78(7):1954–67. https://doi.org/10.1111/jan.15230.
Wu KK, Lopez C, Nichols M. Virtual visits in prenatal care: an integrative review. J Midwifery Womens Health. 2022;67(1):39–52. https://doi.org/10.1111/jmwh.13284.
Alkureishi MA, Lee WW, Lyons M, Press VG, Imam S, Nkansah-Amankra A, Werner D, Arora VM. Impact of Electronic Medical Record use on the patient-doctor relationship and communication: A systematic review. J Gen Intern Med. 2016;31(5):548–60. https://doi.org/10.1007/s11606-015-3582-1.
Farnood A, Johnston B, Mair FS. A mixed methods systematic review of the effects of patient online self-diagnosing in the ‘smart-phone society’ on the healthcare professional-patient relationship and medical authority. BMC Med Inform Decis Mak. 2020;20(1):1–14. https://doi.org/10.1186/s12911-020-01243-6.
Lordon RJ, Mikles SP, Kneale L, Evans HL, Munson SA, Backonja U, Lober WB. How patient-generated health data and patient-reported outcomes affect patient-clinician relationships: A systematic review. Health Informatics J. 2020;26(4):2689–706. https://doi.org/10.1177/1460458220928184.
Noblin A, Hewitt B, Moqbel M, Sittig S, Kinnerson L, Rulon V. Can caregivers trust information technology in the care of their patients? A systematic review. Inform Health Soc Care. 2021;46(1):29–41. https://doi.org/10.1080/17538157.2020.1834399.
Qudah B, Luetsch K. The influence of mobile health applications on patient-healthcare provider relationships: A systematic narrative review. Patient Educ Couns. 2019;102(6):1080–9. https://doi.org/10.1016/j.pec.2019.01.021.
Sunjaya AP, Chris A, Novianti D. Efficacy, patient-doctor relationship, costs and benefits of utilizing telepsychiatry for the management of post-traumatic stress disorder (PTSD): A systematic review. Trends Psychiatry Psychother. 2020;42(1):102–10. https://doi.org/10.1590/2237-6089-2019-0024.
Luo A, Qin L, Yuan Y, Yang Z, Liu F, Huang P, Xie W. The effect of online health information seeking on physician-patient relationships: A systematic review. J Med Internet Res. 2022;24(2):1–20. https://doi.org/10.2196/23354.
Barr N, Vania D, Randall G, Mulvale G. Impact of information and communication technology on interprofessional collaboration for chronic disease management: a systematic review. J Health Serv Res Policy. 2017;22(4):250–7. https://doi.org/10.1177/1355819617714292.
Dalley D, Rahman R, Ivaldi A. Health care professionals’ and patients’ management of interactional practices in telemedicine videoconferencing: a conversation analytic and discursive systematic review. Qual Health Res. 2021;31(4):804–14. https://doi.org/10.1177/1049732320942346.
Irvine A, Drew P, Hower P, Brooks H, Gellatly J, Armitage CJ, Barkham M, McMillan D, Bee P. Are there interactional differences between telephone and face-to-face psychological therapy? A systematic review of comparative studies. J Affect Disord. 2020;265:120–31. https://doi.org/10.1016/j.jad.2020.01.057.
Kazmi Z. Effects of exam room EHR use on doctor-patient communication: a systematic literature review. Inform Prim Care. 2013;21(1):30–9. https://doi.org/10.14236/jhi.v21i1.37.
Nguyen C, McElroy LM, Abecassis MM, Holl JL, Ladner DP. The use of technology for urgent clinician to clinician communications: a systematic review of the literature. Int J Med Inform. 2015;84(2):101–10. https://doi.org/10.1016/j.ijmedinf.2014.11.003.
Rathert C, Mittler JN, Banerjee S, McDaniel J. Patient-centered communication in the era of electronic health records: What does the evidence say? Patient Educ Couns. 2016;100(1):50–64. https://doi.org/10.1016/j.pec.2016.07.031.
Shachak A, Reis S. The impact of electronic medical records on patient-doctor communication during consultation: a narrative literature review. J Eval Clin Pract. 2009;15(4):641–9. https://doi.org/10.1111/j.1365-2753.2008.01065.x.
Wehmann E, Köhnen M, Härter M, Liebherz S. Therapeutic alliance in technology-based interventions for the treatment of depression: Systematic review. J Med Internet Res. 2020;22(6):1–15. https://doi.org/10.2196/17195.
Howard R, Berry K, Haddock G. Therapeutic alliance in psychological therapy for posttraumatic stress disorder: a systematic review and meta-analysis. Clin Psychol Psychother. 2022;29(2):373–99. https://doi.org/10.1002/cpp.2642.
Tapuria A, Porat T, Kalra D, Dsouza G, Xiaohui S, Curcin V. Impact of patient access to their electronic health record: systematic review. Inform Health Soc Care. 2021;46(2):192–204. https://doi.org/10.1080/17538157.2021.1879810.
Irani JS, Middleton JL, Marfatia R, Omana ET, D’Amico F. The use of Electronic Health Records in the exam room and patient satisfaction: a systematic review. J Am Board Fam Med. 2009;22(5):553–62. https://doi.org/10.3122/jabfm.2009.05.080259.
McGinn CA, Grenier S, Duplantie J, Shaw N, Sicotte C, Mathieu L, Leduc Y, Légaré F, Gagnon M. Comparison of user groups’ perspectives of barriers and facilitators to implementing electronic health records: a systematic review. BMC Med. 2011;9(46):1–10. https://doi.org/10.1186/1741-7015-9-46.
Bassi J, Lau F, Lesperance M. Perceived impact of electronic medical records in physician office practices: a review of survey-based research. Interact J Med Res. 2012;1(2):1–23. https://doi.org/10.2196/ijmr.2113.
Nguyen L, Bellucci E, Nguyen LT. Electronic health records implementation: an evaluation of information system impact and contingency factors. Int J Med Inform. 2014;83(11):779–96. https://doi.org/10.1016/j.ijmedinf.2014.06.011.
Mold F, Raleigh M, Alharbi NS, de Lusignan S. The impact of patient online access to computerized medical records and services on Type 2 diabetes: Systematic review. J Med Internet Res. 2018;20(7):1–16. https://doi.org/10.2196/jmir.7858.
Wisner K, Lyndon A, Chesla CA. The electronic health record’s impact on nurses’ cognitive work: an integrative review. 2019;94:74-84. https://doi.org/10.1016/j.ijnurstu.2019.03.003.
Diffin J, Byrne B, Kerr H, Price J, Abbott A, McLaughlin D, O’Halloran P. The usefulness and acceptability of a personal health record to children and young people living with complex health condition: a realist review of the literature. Child Care Health Dev. 2019;45(3):313–32. https://doi.org/10.1111/cch.12652.
Zurynski Y, Ellis LA, Tong HL, Laranjo L, Clay-Williams R, Testa L, Meulenbroeks I, Turton C, Sara G. Implementation of Electronic Health Records in mental health settings: Scoping review. JMIR Ment Health. 2021;8(9):1–15. https://doi.org/10.2196/30564.
Schwarz J, Bärkås A, Blease C, Collins L, Hägglund M, Markham S, Hochwarter S. Sharing clinical notes and Electronic Health Records with people affected by mental health conditions: scoping review. JMIR Ment Health. 2021;8(12):1–17. https://doi.org/10.2196/34170.
Verhoeven F, Tanja-Dijkstra K, Nijland N, Eysenbach G, van Gemert-Pijnen L. Asynchronous and synchronous teleconsultation for diabetes care: a systematic literature review. J Diabetes Sci Technol. 2010;4(3):666–84. https://doi.org/10.1177/193229681000400323.
Brewster L, Mountain G, Wessels B, Kelly C, Hawley M. Factors affecting front line staff acceptance of telehealth technologies: a mixed-method systematic review. J Adv Nurs. 2014;70(1):21–33. https://doi.org/10.1111/jan.12196.
Keijser W, Smits J, Penterman L, Wilderom C. Physician leadership in e-health? A systematic literature review. Leadersh Health Serv (Bradf Engl). 2016;29(3):331–47. https://doi.org/10.1108/LHS-12-2015-0047.
Petit A, Cambon L. Exploratory study of the implications of research on the use of smart connected devices for prevention: a scoping review. BMC Public Health. 2016;16:1–13. https://doi.org/10.1186/s12889-016-3225-4.
Richards R, Kinnersley P, Brain K, McCutchan G, Staffurth J, Wood F. Use of mobile devices to help cancer patients meet their information needs in non-inpatient settings: systematic review. JMIR Mhealth Uhealth. 2018;6(12):1–16. https://doi.org/10.2196/10026.
Watkins JA, Goudge J, Gómez-Olivé FZ, Huxley C, Dodd K, Griffiths F. mHealth text and voice communication for monitoring people with chronic diseases in low-resource settings: a realist review. 2018;3(2):1–15. https://doi.org/10.1136/bmjgh-2017-000543.
Penny RA, Bradford NK, Langbecker D. Registered nurse and midwife experiences of using videoconferencing in practice: a systematic review of qualitative studies. J Clin Nurs. 27(5–6):e739-e752. https://doi.org/10.1111/jocn.14175.
Walker RC, Tong A, Howard K, Palmer SC. Patient expectations and experiences of remote monitoring for chronic diseases: Systematic review and thematic synthesis of qualitative studies. Int J Med Inform. 2019;124:78–85. https://doi.org/10.1016/j.ijmedinf.2019.01.013.
Foong HF, Kyaw BM, Upton Z, Car LT. Facilitators and barriers of using digital technology for the management of diabetic foot ulcers: a qualitative systematic review. Int Wound J. 2020;17(5):1266–81. https://doi.org/10.1111/iwj.13396.
Vimalananda VG, Orlander JD, Afable MK, Fincke BG, Solch AK, Pinne ST, Kim EJ, Cutrona SL, Thomas DD, Strymish JL, Simon SR. Electronic consultations (E-consults) and their outcomes: a systematic review. J Am Med Inform Assoc. 2020;27(3):471–9. https://doi.org/10.1093/jamia/ocz185.
Wickramasekera N, Taylor SK, Lumley E, Gray T, Wilson E, Radley S. Can electronic assessment tools improve the process of shared decision-making? A systematic review. Health Inf Manag J. 2020. https://doi.org/10.1177/1833358320954385.
Thiyagarajan A, Grant C, Griffiths F, Atherton H. Exploring patients’ and clinicians’ experiences of video consultations in primary care: a systematic scoping review. BJGP Open. 2020;4(1):1–8. https://doi.org/10.3399/bjgpopen20X101020.
Ferguson C, Hickman LD, Turkmani S, Breen P, Gargiulo G, Inglis SC. “Wearables only work on patients that wear them”: Barriers and facilitators to the adoption of wearable cardiac monitoring technologies. Cardiovasc Digit Health J. 2021;2(2):137–47. https://doi.org/10.1016/j.cvdhj.2021.02.001.
Scalia P, Durand M, Berkowitz JL, Ramesh NP, Faber MJ, Kremer JAM, Elwyn G. The impact and utility of encounter patient decision aids: Systematic review, meta-analysis and narrative synthesis. Patient Educ Couns. 2019;102(5):817–41. https://doi.org/10.1016/j.pec.2018.12.020.
Yen RW, Smith J, Engel J, Muscat DM, Smith SK, Mancini J, Perestelo-Pérez L, Elwyn G, O’Malley AJ, Leyenaar JK, Mac O, Cadet T, Giguere A, Housten AJ, Langford A, McCaffery K, Durand M. A systematic review and meta-analysis of patient decision aids for socially disadvantaged populations: Update from the International Patient Decision Aid Standards (IDPAS). Med Decis Making. 2021;41(7):870–96. https://doi.org/10.1177/0272989X211020317.
Čartolovni A, Tomičić A, Mosler EL. Ethical, legal, and social considerations of AI-based medical decision-support tools: a scoping review. Int J Med Inform. 2022;161:1–9. https://doi.org/10.1016/j.ijmedinf.2022.104738.
Crooks VA, Agarwal G. What are the roles involved in establishing and maintaining informational continuity of care within family practice? A systematic review. BMC Fam Pract. 2008;9(65). https://doi.org/10.1186/1471-2296-9-65.
Ludwick DA, Doucette J. Adopting electronic medical records in primary care: lessons learned from health information systems implementation experience in seven countries. Int J Med Inform. 2009;78(1):22–31. https://doi.org/10.1016/j.ijmedinf.2008.06.005.
Kruse CS, Argueta DA, Lopez L, Nair A. Patient and provider attitudes toward the use of patient portals for the management of chronic disease: a systematic review. J Med Internet Res. 2015;17(2):1–10.
Crampton NH, Reis S, Shachak A. Computers in the clinical encounter: a scoping review and thematic analysis. J Am Med Assoc. 2016;23:654–65. https://doi.org/10.1093/jamia/ocv178.
Clarke MA, Moore JL, Steege LM, Koopman RJ, Belden JL, Canfield S, Meadows SE, Elliott SG, Kim MS. Health information needs, sources, and barriers of primary care patients to achieve patient-centered care: a literature review. Health Informatics J. 2016;22(4):992–1016. https://doi.org/10.1177/1460458215602939.
Patel MR, Vichich J, Lang I, Lin J, Zheng K. Developing an evidence base of best practices for integrating computerized systems into the exam room: a systematic review. J Am Med Inform Assoc. 2017;24(e1):e207–15. https://doi.org/10.1093/jamia/ocw121.
Palacholla RS, Fischer N, Coleman A, Agboola S, Kirley K, Felsted J, Katz C, Lloyd S, Jethwani K. Provider- and patient-related barriers to and facilitators of digital health technology adoption for hypertension management. JMIR Cardio. 2019;3(1):1–12. https://doi.org/10.2196/11951.
Davies F, Shepherd HL, Beatty L, Clark B, Butow P, Shaw J. Implementing web-based therapy in routine mental health care: Systematic review of health professionals’ perspectives. J Med Internet Res. 2020;22(7):1–12. https://doi.org/10.2196/17362.
Hilty DM, Torous J, Parish MB, Chan SR, Xiong G, Scher L, Yellowlees PM. A literature review comparing clinicians’ approaches and skills to in-person, synchronous, and asynchronous care: Moving towards competencies to ensure quality care. 2021;27(4):356-373. https://doi.org/10.1089/tmj.2020.0054.
Giordan LB, Tong HL, Atherton JJ, Ronto R, Chau J, Kaye D, Shaw T, Chow C, Laranjo L. The use of mobile apps for heart failure self-management: Systematic review of experimental and qualitative studies. JMIR Cardio. 2022;6(1):1–18. https://doi.org/10.2196/33839.
Duea SR, Zimmerman EB, Vaughn LM, Dias S, Harris J. A guide to selecting participatory research methods based on project and partnership goals. J Particip Res Methods. 2022;3(1):1–32. https://doi.org/10.35844/001c.32605.
Daniel H, Sulmasy LS. Policy recommendations to guide the use of telemedicine in primary care settings: An American College of Physicians position paper. Ann Intern Med. 2015;163(10):787–98. https://doi.org/10.7326/M15-0498.
Husain L, Greenhalgh T, Hughes G, Finlay T, Wherton J. Desperately seeking the intersectionality in digital health disparities research: Narrative review to inform a richer theorisation of multiple disadvantage. J Med Internet Res. 2022;24(12):1–23. https://doi.org/10.2196/42358.
Pinto RF, Ferreira ML, Oliveira VC, Franco MR, Adams R, Maher CG, Ferreira PH. Patient-centred communication is associated with positive therapeutic alliance: a systematic review. J Physiother. 2012;58(2):77–87. https://doi.org/10.1016/S1836-9553(12)70087-5.
Hajesmaeel-Gohari S, Khordastan F, Fatehi F, Samzadeh H, Bahaadinbeigy K. The most used questionnaires for evaluating satisfaction, usability, acceptance, and quality outcomes of mobile health. BMC Med Inform Decis Mak. 2022;22:1–9. https://doi.org/10.1186/s12911-022-01764-2.
Scott CPR, Wildman JL. Culture, communication, and conflict: A review of the global virtual team literature. In: Wildman JL, Griffith RL, editors. Leading global teams: Translating multidisciplinary science to practice. New York: Springer; 2015. p. 13–32.
Hacker J, Johnson M, Saunders C, Thayer AL. Trust in virtual teams: a multidisciplinary review and integration. Australas J Inf Syst. 2019;23:1–36. https://doi.org/10.3127/ajis.v23i0.1757.
Meluso J, Johnson S, Bagrow J. Flexible environments for hybrid collaboration: Redesigning virtual work through the four orders of design. Des Issues. 2022;38(1):55–69. https://doi.org/10.1162/desi_a_00670.
Pham MT, Rajić A, Greig JD, et al. A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371–85. https://doi.org/10.1002/jrsm.1123.
Acknowledgements
The authors would like to thank Alana Armas for her expertise and assistance during the early stages of conceptualising this review and developing the search strategy.
Funding
Primary funding for this research was through the AMS Healthcare Fellowship in AI/Digital Health and Compassion program. As well, this research was undertaken, in part, thanks to funding from the Canada Research Chairs Program.
Author information
Authors and Affiliations
Contributions
MR: Conceptualisation, methodology, project administration, writing – original draft preparation, review and editing; CB: Methodology, writing – review and editing; DW: Writing – review and editing; RU: Writing – review and editing; CSG – Conceptualisation, methodology, project administration, writing – review and editing.
Authors’ information
CSG, RU and DW all have expertise in primary care research, digital health, compassionate care, and the evidence synthesis methods used in this study. CSG holds a Tier 2 Canada Research Chair in Implementing Digital Health Innovation. She previously held a 2020–2021 AMS Healthcare Fellowship in Compassion and Artificial Intelligence and Digital Health through which she conducted ethnographic research to understand how trust-based relationships, needed for compassionate care, can be built (or prevented) through digital health tools. RU has previously held a Canada Research Chair in Primary Care (2005–2015) and is also a primary care clinician. DW is a compassionate care expert, and his work focuses on exploring the role of digital technologies in supporting patient partnership and co-designing technologies to promote compassionate care.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Search strategy.
Additional file 2.
Impact of technology on patient-provider relationships.
Additional file 3.
Impact of technology on provider-provider relationships.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ramachandran, M., Brinton, C., Wiljer, D. et al. The impact of eHealth on relationships and trust in primary care: a review of reviews. BMC Prim. Care 24, 228 (2023). https://doi.org/10.1186/s12875-023-02176-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-023-02176-5